What to expect
NeoGenomics is a participating provider with Medicare and Medicaid, in addition to many private insurance providers and managed care organizations.
NeoGenomics clients receive an itemized invoice that includes the date, patient’s name, accession number, test(s) performed, and test fees for each specimen completed during a given month. Please note that these invoices are payable upon receipt. If you have any questions pertaining to your account, please contact our Billing team immediately so that we may resolve them in a timely manner.
For providers who choose third-party billing, NeoGenomics will bill the patient’s insurance provider in accordance with their healthcare plan. We will work closely with your office to obtain the necessary medical documentation, including ICD-10 codes, and handle all appeals to minimize the impact for your patient.
Billing resources for clients
ICD-10 code resources
BCRABL, JAK2, CALR, MPL
MolDX: Genetic Testing for BCR-ABL Negative Myeloproliferative Disease
BRAF
MolDX: FDA-Approved BRAF Tests
KRAS
MolDX: FDA-Approved KRAS Tests
EGFR
MolDX: FDA-Approved EGFR Tests
NGS for Solid Tumors
MolDX: Next-Generation Sequencing for Solid Tumors
NRAS
MolDX: NRAS Genetic Testing
Flow Cytometry
Lab: Flow Cytometry
Cytogenetics
CMS Manual System
NCD190.3 Cytogenetics Studies
Prior authorization support for molecular & genetic testing
Molecular and genetic testing is an evolving field in oncology diagnostics, and many insurance providers have established a policy of prior authorization before testing can be performed to ensure appropriate use. NeoGenomics contracts with many national and regional healthcare insurance plans to help offer affordable testing to our patients and clients; however, each insurance plan may have a different process for obtaining prior authorization for testing.
For more specific information, NeoGenomics recommends calling the patient’s insurance plan for their current policy. For any questions or prior authorization support, please email
priorauthorizations@neogenomics.com.
Pay your bill
NeoGenomics offers convenient options to pay your bill

Online payment
Pay online through our ilab Client Portal; for access, please email us with your client name and number.
Credit or debit
You may complete the form on your invoice and return it to us using the instructions provided on the invoice. Or, to pay by phone, please call us at 866.776.5907, Option 2. A receipt can be mailed to you upon request.
Check or money order
Make the check or money order payable to NeoGenomics Laboratories, and mail it to:
NeoGenomics Laboratories, Inc.
P.O. Box 947403
Atlanta, GA 30394-7403
Pay your bill online
Insurance coverage
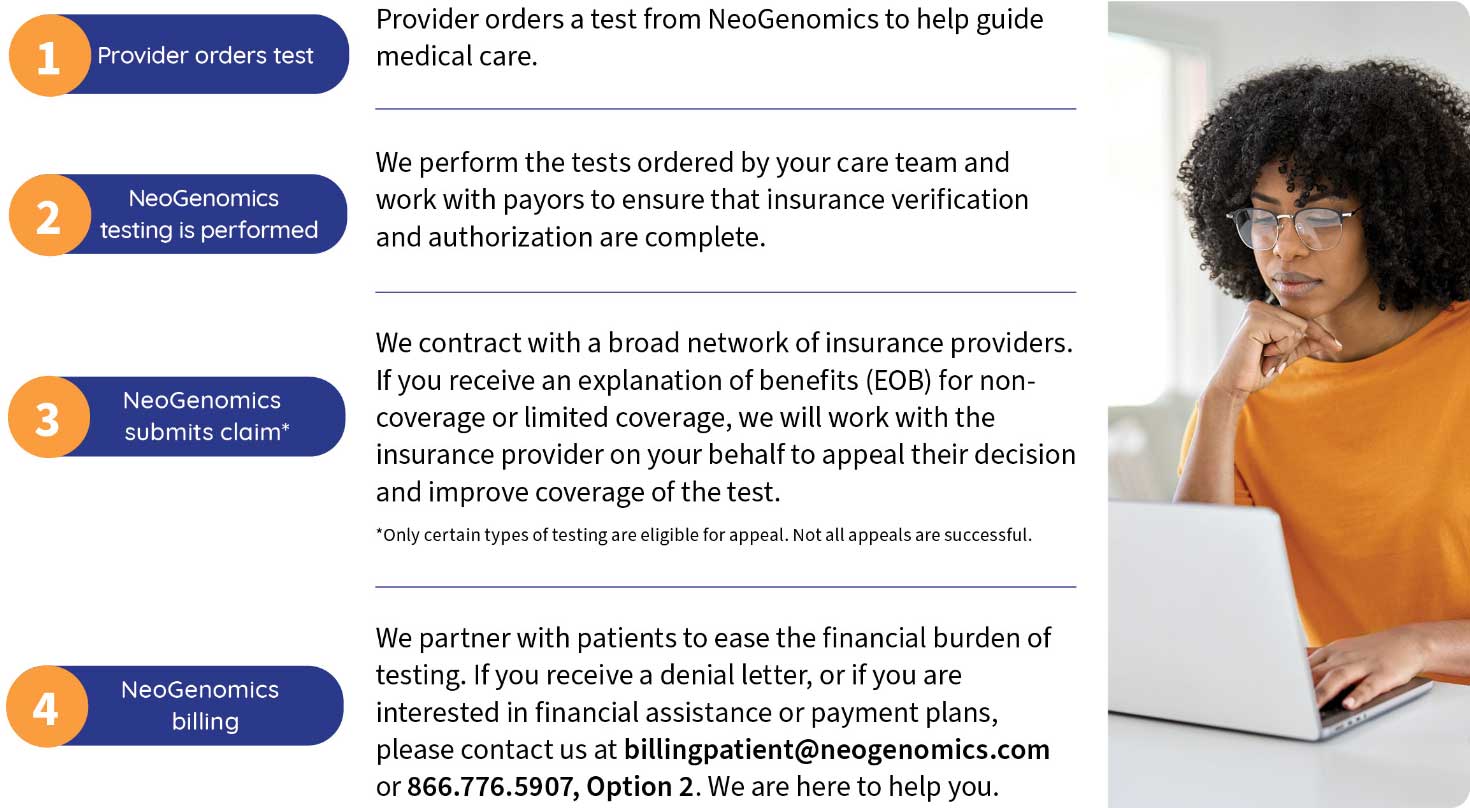
NeoGenomics is committed to working with patients and their insurance providers to ensure that everyone has access to high-quality cancer testing.
We believe that all patients, regardless of socioeconomic status, ethnicity, or race, should have the same access to care. This is why NeoGenomics is proud to be in-network with hundreds of national health insurance providers and programs, covering over 300 million lives in the United States.
NeoGenomics partners with patients to ease the financial burden of testing. If you receive a denial letter, or if you are interested in financial assistance or in setting up a payment plan, please contact us.
Billing process
Billing FAQs
NeoGenomics contracts with many national and regional insurance providers.
NeoGenomics strives to make cancer testing affordable and accessible to all. To that end, we offer payment plans and discounts for prompt pay. Please call our Billing team for more information: 866.776.5907, Option 2.
We can work on your behalf with your insurer to appeal against their initial decision, to try to improve your coverage for the test.
An EOB, or explanation of benefits, is a document from your insurance provider that shows the details of a claim submitted for a medical service. It is not a bill, but an explanation from the insurance provider regarding anticipated cost sharing for the service.
Yes. We offer financial assistance options that can help make your cancer care more affordable, are in line with federal regulations, and are based on income.
We offer convenient options for paying your bill.
Pay online
Pay by phone: 866.776.5907, Option 2
Billing resources for patients
Financial assistance program
We believe that every patient should have access to the best possible cancer care. We have a dedicated support team to assist with insurance appeals, prior authorizations, and financial assistance including interest-free payment plans. Both insured and uninsured patients may qualify for no-cost or reduced-cost testing through our billing resource programs. We also offer prompt-pay discounts and payment plans.
How to apply for financial assistance
Our online financial assistance application is currently unavailable, but you can still apply using the forms below. If you need assistance, please contact our Billing specialists at 866.776.5907, Option 2.
You can also apply by mail. Simply download, print, and complete your application and mail it to:
NeoGenomics Laboratories, Inc.
P.O. Box 947586
Atlanta, GA 30394-7586
Financial Assistance Application (English)
Financial Assistance Application (Spanish)
Once your application is received, a Patient customer service representative will contact you within 48 hours.